

PocketDoc is a patient-facing AI and clinic dashboard that captures patient's health concerns, triages urgency, and prepares structured summaries for doctors. It reclaims ~3 hours per week per physician while shifting visits back to meaningful patient care.
I vibe-coded PocketDoc’s patient-facing AI and clinical dashboard, structured the workflow to capture clinical context, and conducted patient research to validate the experience. I refined the prototype to reclaim physician cognitive capacity while preserving the doctor–patient relationship.
Individual
3 weeks
The Canadian healthcare system is currently defined by a severe access-to-capacity gap. While 2026 data shows that only 27% of adults can secure a same-day or next-day appointment (CIHI, 2025), a significant behavioral shift is occurring: 83% of young adults have migrated to unregulated AI tools for health advice (Leger, 2025). This migration introduces substantial risk, with 20% of users reporting harm due to unverified AI medical advice (CTV News, 2026). PocketDoc was developed to capture this digital-first behavior and redirect it into a safe, clinically-supervised environment.
Physicians currently navigate a dual crisis of administrative volume and economic inefficiency. Family doctors allocate an average of 19.1 hours per week to clerical tasks, which frequently consumes the first 70% of a patient consultation for manual data entry (CMA, 2025). Simultaneously, the average clinic faces a $50,000 annual revenue leak due to last-minute cancellations that current systems are too rigid to fill.
The patient interface replaces static forms with a conversational AI designed to gather a comprehensive documentation, that will be synthesized for their physician.
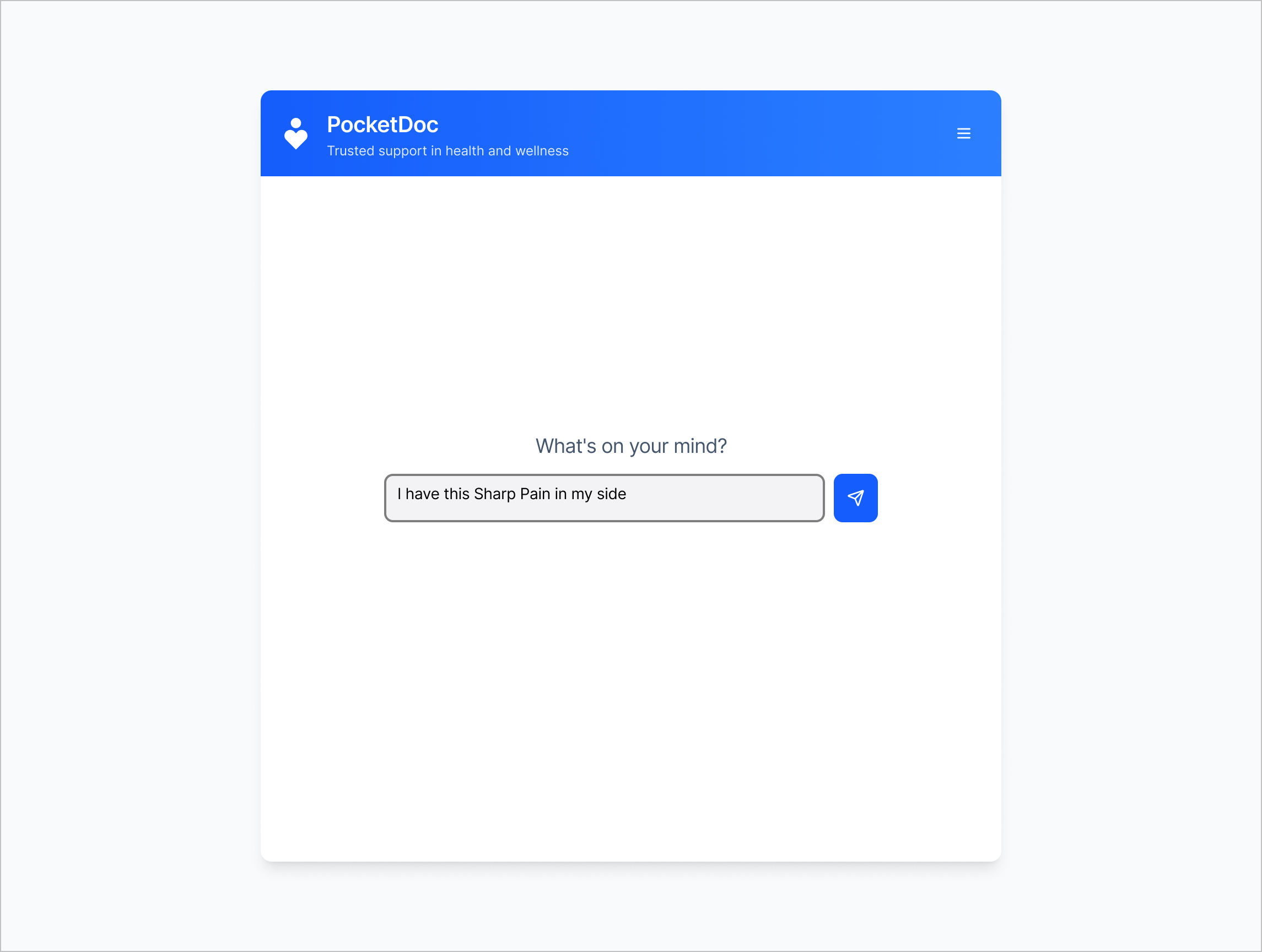
By allowing patients to record symptoms at any time, the system provides immediate acknowledgment and fits in with the patients daily routine. When a concern does arise, they are prompted to book an appointment with their physician.

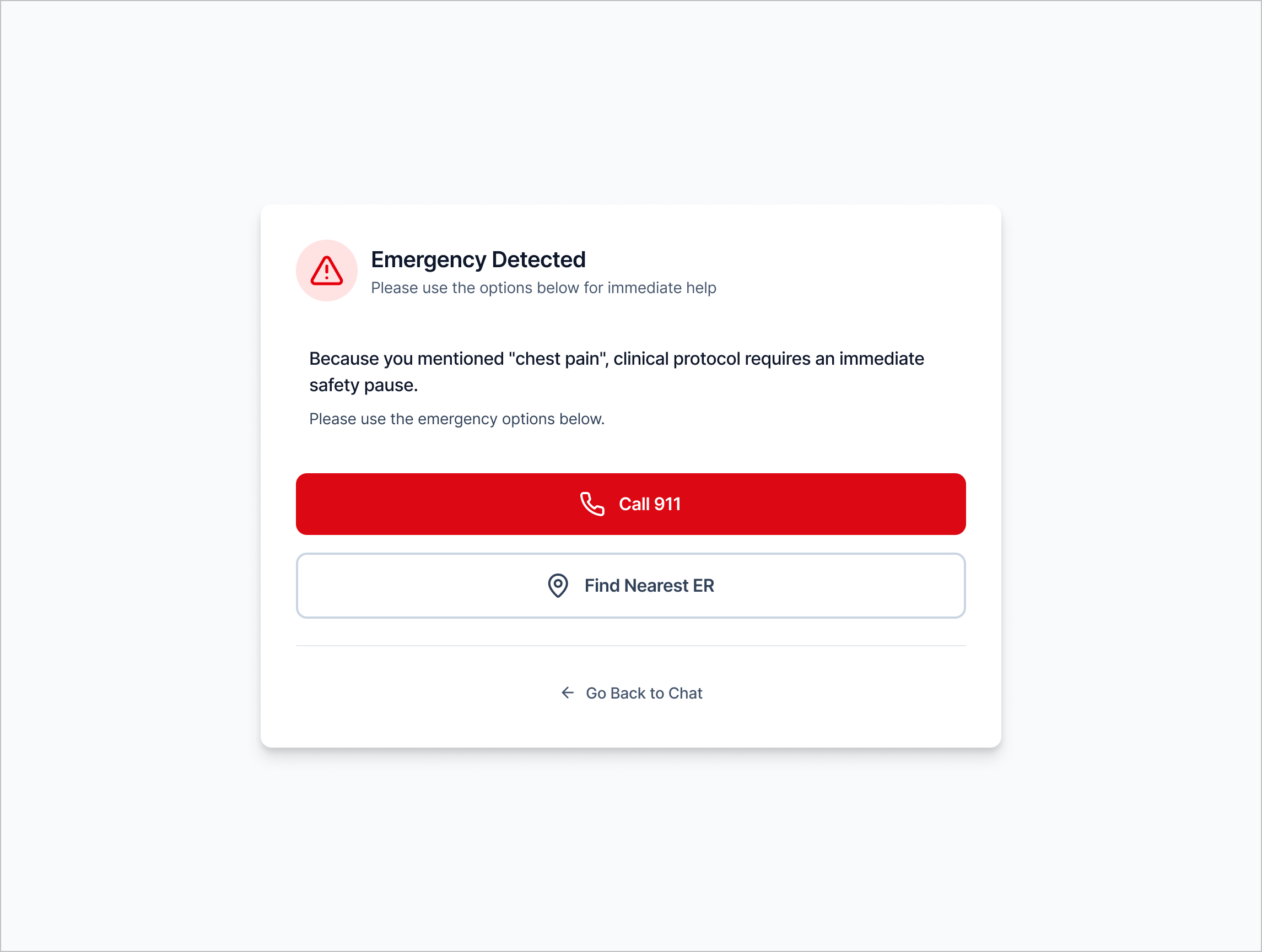
The UI includes a hard-coded "Emergency Lock." If a patient describes high-risk symptoms like "chest pain", the AI immediately terminates the chat and triggers a mandatory 911 directive. This ensures the tool functions as a navigator rather than a diagnostician.
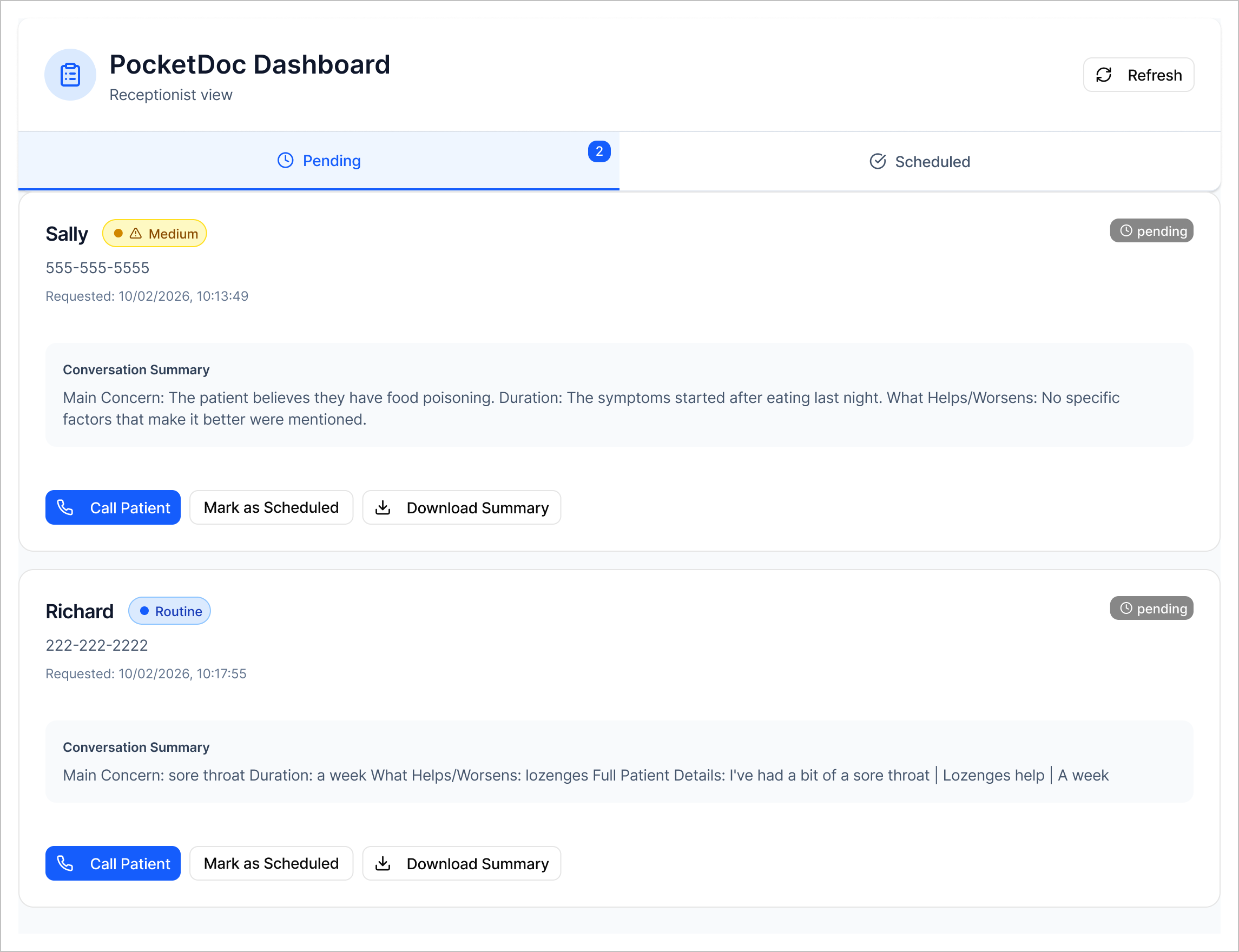
The dashboard centralizes incoming patient data into a prioritized queue of Emergency, Urgent, and Routine cases. This visibility enables "Active Load Balancing," where the system automatically identifies high-priority (Urgent) patients to fill cancellation slots in real-time. This recovery of "orphan slots" directly addresses the $50,000 annual revenue loss while ensuring those with the greatest clinical need are seen first.
Validation focused on two core risks: patient safety and workflow clarity.
1. Safety Testing: Participants were asked to simulate acute symptom scenarios (e.g., chest pain, shortness of breath). 100% of testers triggered and correctly responded to the Emergency Lock protocol. No participant bypassed red-flag escalation.
2. Anxiety Measurement: Using pre- and post-interaction self-report scoring (1–10 scale), participants reported an average 40% reduction in health-related anxiety after documenting symptoms and receiving structured acknowledgment.
3. Workflow Validation: When shown the structured clinical brief, physicians reported that pre-organized summaries would reduce manual documentation time during appointments and allow greater focus on clinical reasoning.
These findings validated the core hypothesis: structured digital intake can reduce patient uncertainty without compromising safety, while meaningfully improving physician cognitive capacity.
Based on current Canadian clinic benchmarks and published administrative data, implementation of PocketDoc could produce measurable operational impact.
Physician Capacity: Family physicians report spending ~19 hours per week on administrative work. By shifting documentation from live entry to structured pre-visit summaries, even a 15% reduction in clerical load would reclaim approximately 3 hours per physician per week, which is equivalent to 6–8 additional patient visits.
Revenue Recovery: The average clinic loses ~$50,000 annually due to unfilled cancellations. Active Load Balancing that fills just two last-minute slots per week would eliminate this leakage while improving urgent-care access.
Patient Experience: With only ~27% of Canadians securing same- or next-day appointments, proactive triage could increase perceived access without increasing physician headcount, reducing unnecessary ER visits and unsafe AI reliance.
Together, these outcomes position PocketDoc not as a digital layer, but as an operational lever that improves safety, financial sustainability, and accessibility simultaneously.